Gut-brain talk: Three amino acids linked to appetite loss during illness
Key takeaways
- Researchers found that ill mice, in a catabolic state, avoid protein-rich foods due to their aversion of three specific amino acids — glutamine, lysine, and threonine.
- These three amino acids produce higher levels of ammonia, which is detected in the small intestine via a receptor and signaled to the brainstem.
- The study offers a new insight into appetite suppression during illness, potentially leading to therapeutic approaches for managing appetite in various conditions.
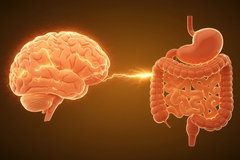
Researchers have investigated the phenomenon of appetite loss during illness, discovering that mice in a similar catabolic state are strongly averse to protein-rich foods. They link this aversion to specific amino acids that produce higher levels of ammonia and lower appetite through a gut-to-brain signaling pathway.
“The hope is that, down the line, we’re able to develop therapeutic approaches to support the recovery process,” says Nikolai Jaschke, co-first author of the study and a principal investigator and physician at the Hamburg Center for Translational Immunology and University Medical Center Hamburg-Eppendorf, Germany.
Jaschke stresses there is a lack of therapeutic tools to support sick patients with reduced appetite.

Investigating the catabolic state
As a result of lower food intake, a sick person’s body will begin breaking down complex molecules like protein and carbohydrates for energy. The scientists began their study by looking into this catabolic state, which occurs during illness, fasting, stress, or intense exercise.
In the study published in Cell, researchers offered mice in a catabolic state one of three diets that each had the same amount of calories and micronutrients but different macronutrients: protein, carbohydrates, or fat.
Mice fed the high-carbohydrate and high-fat diets ate expected amounts. However, those on the protein-rich diet ate significantly less than mice not in a catabolic state.
Because people typically eat less while they’re sick, hospital caregivers usually offer them high-protein meals to help replace the protein they lose. However, the researchers point to two recent clinical trials that found that consuming extra protein during recovery worsened patient outcomes instead of making them better.
The study team tested 20 different amino acids to see if any would lead to the same reduction in food intake. They discovered only three that did — glutamine, lysine, and threonine. Catabolic mice given foods without these three amino acids ate without problems.
The role of ammonia
The scientists explain that protein — whether stored in tissue or consumed in the diet — breaks down and generates ammonia that needs to be detoxified by the liver and excreted by the kidneys. Because this process requires water, it increases urination.
The researchers found that the three amino acids led to higher ammonia levels than other amino acids. Moreover, mice were able to eat more protein-rich food when their ability to detoxify ammonia increased.
“I was giving mice the high-protein diet for a longer period of time to see if their appetites for it would change over time, and they did. The mice slowly increased how much of it they ate,” says Jaschke.
“But then I noticed their cage bedding was very wet and figured that their water bottles were leaking. It turned out to be urine, and the mice were urinating more than ten times the amount they typically do.”
These observations led to the conclusion that the mice were self-adjusting their intake of amino acids based on their capacity to detoxify ammonia.
“It’s still not clear why they’re more ammoniogenic, but our findings collectively suggest that this generation of ammonia is necessary and sufficient for the protein aversion we observed in the catabolic mice,” notes Jaschke.
Gut-brain talk to suppress appetite
The scientists identified that ammonia production was being sensed in a part of the small intestine called the duodenum. A specific receptor on a particular type of cell was responsible for this task.
When the researchers developed mice without the receptor, these animals were not averse to food rich in glutamine, lysine, and threonine. Alternatively, activating the receptor strongly suppressed food intake.
“With this being a behavior, it has to be controlled in some way by the brain, so we started looking for which brain areas might be involved,” elaborates Joseph Luchsinger, M.D., Ph.D., co-first author of the study and a resident in Yale School of Medicine’s Neuroscience Research Training Program.
The team pinpointed two regions in the brainstem connected to protein intake and ammonia production — the area postrema and the nucleus tractus solitarius. These regions relate to satiety and nausea and are already targeted pharmacologically by weight loss drugs like semaglutide (such as in Ozempic medication) for appetite suppression.
The researchers found that neurons in the duodenum are found in part of the vagus nerve, the bundle of sensory fibers that delivers information from organs like the intestines to the brainstem.
When the researchers silenced these duodenum neurons, mice ate more protein. “The findings indicate that during illness recovery, this gut-to-brain signaling is able to detect harmful ammonia before it begins to circulate in the blood and suppress protein appetite,” they detail.
There is still more to uncover, but the researchers note the findings are intriguing. For instance, when they counteracted the various parts of this system, mice never over-ate protein, suggesting there are additional layers of regulation to identify.
Designing future recovery diets
More research needs to be done to see if these observations translate to humans. The study authors also suggest follow-up research may identify a more effective recovery diet for sick patients.
Luchsinger highlights potential applications in his field. “How and why we choose to eat is really poorly understood. And it’s significantly altered in psychiatric illness, from depression and anxiety to anorexia, but we don’t yet know why that is.”
Luchsinger is curious how Jaschke’s findings might relate to psychiatric illnesses, particularly those that currently lack medications.
“The next step is to compare different diets across different physiological and disease states to see whether reducing the amount of these three amino acids might promote illness recovery,” says Jaschke.
“And this would be relevant for people with urea cycle disorders, for suppressing overactive appetite, and for stimulating appetite when it’s pathologically suppressed, such as with anorexia or cancer cachexia.”














